Polycystic Ovary Syndrome and Endometriosis
Introduction:
What is Polycystic Ovary Syndrome(PCOS) and Endometriosis. Women’s reproductive health is a complex and integral part of their overall well-being. Two
conditions, Polycystic Ovary Syndrome (PCOS) and Endometriosis, significantly impact
fertility and general health, yet are often misunderstood. While these conditions are distinct in
their causes and manifestations, they share some common symptoms, such as pelvic pain and
irregular periods, which can lead to delayed diagnosis and treatment.
In this blog, we will delve into the details of PCOS and Endometriosis, exploring their
symptoms, causes, diagnosis, treatments, and how they affect fertility. We’ll also cover lifestyle
changes and medical interventions to manage these conditions and highlight how they are
connected in broader discussions about reproductive health.
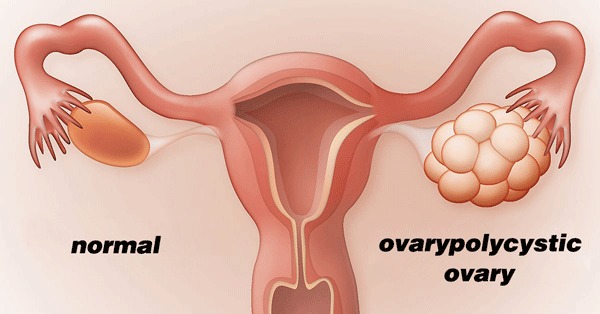
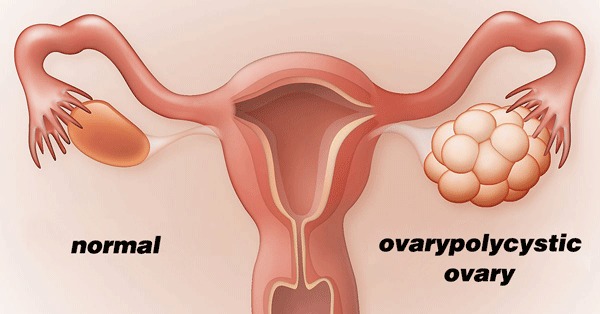
Section 1: What is Polycystic Ovary Syndrome (PCOS)?
Polycystic Ovary Syndrome is one of the most common hormonal disorders affecting women
of reproductive age. Characterized by a combination of symptoms, PCOS can lead to long-term
health issues, including infertility, diabetes, and cardiovascular diseases.
1.1 Symptoms of PCOS
The symptoms of PCOS vary from woman to woman, but the most common signs include:
- Irregular periods: Fewer or absent menstrual cycles, or cycles that are longer than normal.
- Excess androgen: Elevated levels of male hormones, which may result in physical signs
- like excess facial and body hair (hirsutism), severe acne, or thinning hair.
- Polycystic ovaries: Enlarged ovaries with numerous small cysts visible during an ultrasound.
Other associated symptoms include:
- Weight gain or difficulty losing weight
- Insulin resistance (which can lead to type 2 diabetes)
- Skin conditions such as darkening of the skin or skin tags.
1.2 Causes of PCOS
The exact cause of PCOS is not well understood, but several factors are thought to play a role, including:
- Genetics: PCOS tends to run in families, indicating a genetic link.
- Insulin resistance: Many women with PCOS have elevated insulin levels, which may lead to increased androgen production by the ovaries.
- Hormonal imbalances: PCOS is often associated with elevated levels of androgens (male hormones) and low levels of progesterone, which disrupts normal ovulation.
1.3 Diagnosis of PCOS
To diagnose PCOS, doctors typically look for at least two of the following criteria:
- Irregular or absent periods
- Elevated androgen levels
- Ovaries that appear polycystic on ultrasound.
Tests may include blood work to measure hormone levels, a pelvic exam, and an ultrasound to visualize the ovaries.
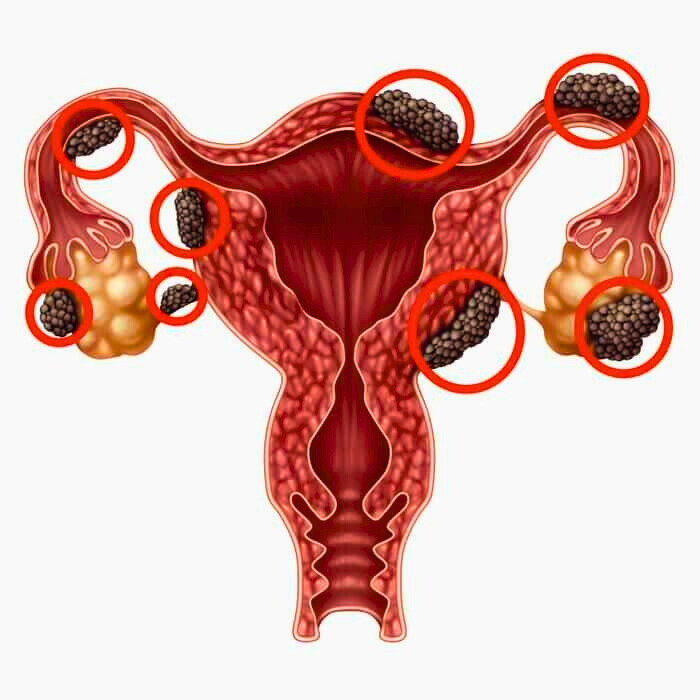
 section 2: what is endometriosis?
section 2: what is endometriosis?
Endometriosis is a chronic condition in which tissue similar to the lining of the uterus
(endometrium) grows outside the uterus. This misplaced tissue causes inflammation, scarring,
and adhesions, often leading to chronic pain and fertility problems.
2.1 Symptoms of Endometriosis
Endometriosis presents differently in each woman, but common symptoms include:
- Chronic pelvic pain: Often correlating with menstrual cycles but can occur at any time.
- Pain during intercourse (dyspareunia]
- Painful periods (dysmenorrhea)
- Heavy menstrual bleeding or bleeding between periods
- Infertility
Other less common symptoms include digestive issues like diarrhea, constipation, or bloating, particularly during menstruation.
2.2 Causes of Endometriosis
The exact cause of endometriosis is unknown, but there are several theories:
- Retrograde menstruation: Menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body.
- Genetic factors: Endometriosis can run in families, suggesting a genetic predisposition
- Immune system disorders: Problems with the immune system may make the body unable to recognize and destroy endometrial-like tissue growing outside the uterus.
2.3 Diagnosis of Endometriosis
Endometriosis is often difficult to diagnose because its symptoms can mimic other conditions. Diagnosis usually involves:
- Pelvic exams
- Ultrasound: Though it cannot definitively diagnose endometriosis, it can identify cysts associated with the condition.
- Laparoscopy: A surgical procedure where a camera is inserted into the pelvic cavity to visually confirm the presence of endometrial tissue outside the uterus.
Section 3: How PCOS and Endometriosis Affect Fertility
Both PCOS and endometriosis can contribute to infertility, but they do so in different ways.
3.1 PCOS and Infertility
Women with PCOS may have difficulty getting pregnant due to irregular or absent ovulation.
Without regular ovulation, there are fewer chances for an egg to be fertilized. Even if ovulation
occurs, hormonal imbalances can make it difficult for the lining of the uterus to support implantation.
3.2 Endometriosis and Infertility
Endometriosis can cause fertility problems in several ways:
- The inflammation caused by endometriosis may damage the sperm or egg or interfere with their ability to meet and fertilize.
- Scar tissue from endometriosis can block the fallopian tubes, preventing the egg from reaching the uterus.
- Endometriosis may also affect the uterine lining, making it harder for a fertilized egg to implant.
Section 4: Treatment Options for PCOS and Endometriosis
4.1 Treating PCOS
There is no cure for PCOS, but several treatments can help manage the symptoms and improve fertility:
- Lifestyle changes: Diet and exercise can help manage weight and improve insulin sensitivity, which may restore normal ovulation.
- Medications: Birth control pills can regulate periods, while metformin can help manage insulin resistance. Fertility drugs, such as Clomid, may help stimulate ovulation.
- Surgery: In some cases, laparoscopic ovarian drilling may be recommended to help restore ovulation.
4.2 Treating Endometriosis
Endometriosis treatment focuses on managing pain and improving fertility:
- Pain relief: Over-the-counter pain medications or hormonal treatments (e.g., birth control pills, GnRH agonists) may help control pain.
- Surgery: In severe cases, laparoscopic surgery can remove endometrial implants and scar tissue, improving pain and fertility outcomes.
- Fertility treatments: Assisted reproductive technologies like In Vitro Fertilization (IVF) may be needed if endometriosis has severely affected fertility.
Section 5: The Role of Lifestyle in Managing PCOS and Endometriosis
Lifestyle plays a significant role in managing both conditions. Here are key factors that may help:
5.1 Diet and Nutrition
- A low glycemic index (GI) diet can help regulate blood sugar levels in women with PCOS, reducing symptoms like weight gain and irregular periods.
- For women with endometriosis, an anti-inflammatory diet rich in omega-3 fatty acids, fruits, and vegetables may help reduce inflammation and pain.
5.2 Exercise and Weight Management
- Regular physical activity can help women with PCOS improve insulin sensitivity and manage weight.
- In women with endometriosis, gentle exercise such as yoga and stretching can help reduce pain and improve overall well-being.
Section 6: Psychological and Emotional Impact of PCOS and Endometriosis
Both PCOS and endometriosis can take an emotional toll due to the chronic pain, infertility
challenges, and physical symptoms like weight gain or hair loss. Depression, anxiety, and stress
are common among women with these conditions.
6.1 Coping Strategies
- Support groups: Connecting with others who have similar experiences can provide emotional support.
- Counseling: Professional therapy can help address the mental and emotional challenges associated with these conditions.
 Conclusion: Managing PCOS and Endometriosis for a Better Quality of Life
Conclusion: Managing PCOS and Endometriosis for a Better Quality of Life
While PCOS and endometriosis are chronic conditions that require ongoing management, many
women are able to lead fulfilling lives with the right treatment and lifestyle modifications.
Whether the goal is to manage pain, regulate menstrual cycles, or achieve pregnancy,
understanding these conditions and seeking appropriate care is key to improving health outcomes.
If you suspect you have PCOS or endometriosis, it’s essential to consult a healthcare
professional for proper diagnosis and treatment. With the right approach, it’s possible to manage
the symptoms and minimize their impact on daily life.